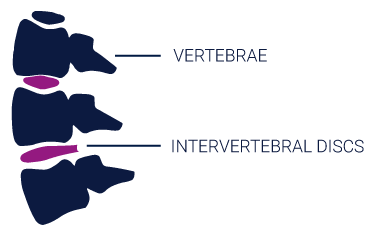
The spine is composed of two main structural components: (1) vertebrae and (2) intervertebral discs.
- The vertebrae are the bones of the spine that function to protect the spinal cord and support the upper body.
- Each vertebra is separated by an intervertebral disc which acts to cushion against impact and provide flexibility to support your body’s ability to bend and rotate.1
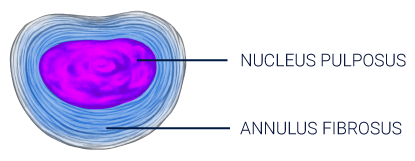
The intervertebral disc (IVD) consists of three regions, the annulus fibrosus (AF), the nucleus pulposus (NP) and the cartilaginous endplate.2
- The annulus fibrosus is a fibrous outer ring of collagen fibers that functions as the primary load-bearing component of the IVD.3
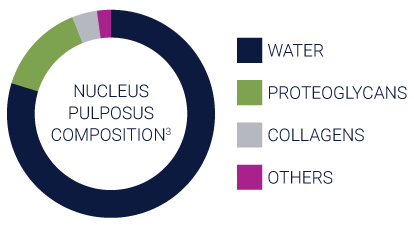
- The nucleus pulposus is a hydrophilic gelatinous core comprised primarily of proteoglycans, collagen II, water, and cells. Healthy nucleus pulposus contains ~80% water, and the high water content provides the mechanical function of absorption and redistribution of spinal loads.4, 5
- The endplates permit diffusion and provide the main source of nutrition for the disc.6
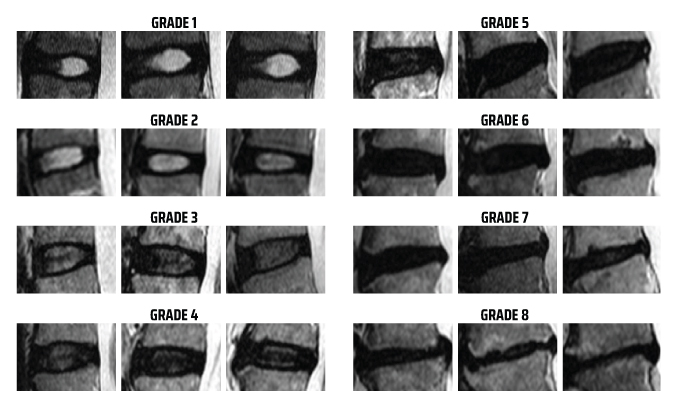
Nutrition, genetics, environmental factors, lifestyle, and any prior injury can all play a role in the induction and future progression of intervertebral disc degeneration. Degeneration typically begins within the nucleus pulposus (NP). Over time, the NP becomes less efficient in its ability to absorb physiological loads, which may be associated with reduced volume of NP within the disc.
The lumbar spine carries a significant weight-bearing function and supports substantial rotational and translational movement, making the area susceptible to degeneration and subsequent pain. One of the most common causes of chronic low back pain (CLBP) is disc degeneration, affecting approximately 40% of CLBP patients.7 Functionally, discogenic pain is exacerbated by mechanical loading and axial rotation of the spine, as these positions maximize biomechanical stresses.
Non-surgical management involves non-invasive treatments for low back pain to temporarily alleviate pain and manage discomfort.
Physical Therapy
May include coordination, strengthening, and endurance therapy to improve flexibility and range of motion.
Chiropractic Treatment
May include acupuncture, massage, spinal manipulation, or mobilization therapy to manage symptoms and maintain functionality.
Pharmaceutical Pain Management
May include prescribed acetaminophen, NSAIDS, skeletal muscle relaxants, antidepressants, antiepileptic drugs, benzodiazepines, tramadol, opioids and/or systemic corticosteroids.
Intermediate treatments may be considered before more invasive treatments to manage pain and provide temporary relief through interventional techniques.
Radio Frequency Ablation (RFA)
Procedure that involves heating a pain-stimulating nerve to create a heat lesion, preventing the nerve from sending pain signals to the brain.
Epidural Steroid injections (ESI)
Injection of a steroid into the epidural space to manage acute pain and provide temporary relief.
Medial Branch Block
A spinal injection to temporarily block the pain signals coming from the medial nerves. A medial branch block can provide temporary pain relief.
Surgical interventions may be necessary for patients who have failed traditional non-surgical management treatments and continue to experience persistent pain and/or weakness.
Lumbar Fusion
Surgical procedure designed to restrict motion at a painful vertebral segment through the joining of adjacent vertebrae.
Lumbar Disc Replacement
Replacement of a degenerated disc with a synthetic disc designed to preserve motion in the affected vertebral segment.
Nucleus Replacement
Replacement of the degenerated nucleus pulposus with a silicone material in an effort to preserve the annulus fibrosus via weight redistribution and recreation of physiological motion.
- Zhu, Qiaoqiao: Numerical Modeling of Intervertebral Disc Degeneration and Repair (2016). Open Access Dissertations. Paper 1594.
- Walter BA, Torre OM, Laudier D, Naidich TP, Hecht AC, Iatridis JC. Form and function of the intervertebral disc in health and disease: a morphological and stain comparison study. J Anat. 2015;227(6):707–716
- Lundon K, Bolton K. Structure and Function of the Lumbar Intervertebral Disk in Health, Aging, and Pathologic Conditions. J Orthop Sports Phys Ther. 2001;31(6):291-306.
- Chen S, Fu P, Wu H, Pei M. Meniscus, articular cartilage and nucleus pulposus: a comparative review of cartilage-like tissues in anatomy, development and function. Cell Tissue Res. 2017;370(1):53–70.
- Iatridis J et al. Measurements of Proteoglycan and Water Content Distribution in Human Lumbar Intervertebral Discs (2007); SPINE; 32(14): 1493-97
- Adams MA, McNally DS, Dolan P. 1996. Stress’ distributions inside intervertebral discs. The effects of age and degeneration. J Bone Joint Surg Br 78-B:965–972.
- Bogduk,N. The Lumbar Disc and Low Back Pain. Neurosurg. Clin.N.Am.1991,2,791–806.
- Griffith, J. F., Wang, Y. X., Antonio, G. E., Choi, K. C., Yu, A., Ahuja, A. T., & Leung, P. C. (2007). Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine, 32(24), E708–E712. https://doi.org/10.1097/BRS.0b013e31815a59a0
- Bogduk N, Aprill C, Derby R. Lumbar discogenic pain:state-of-the-art review. Pain Med. 2013;14(6):813-836.doi:10.1111/pme.12082

